Healthcare billing is a high-stakes balancing act. Providers need to be compensated fairly for the services they deliver, insurers need transparency and accuracy, and patients need to understand what they’re being billed for. Nowhere is this more challenging—or more crucial—than in the realm of inpatient care. At the heart of this process are inpatient billing codes, the structured identifiers that translate complex clinical activities into billable items.
For hospitals and healthcare systems, understanding and using inpatient billing codes correctly can mean the difference between financial stability and revenue loss. Mistakes aren’t just inconvenient—they can trigger claim denials, compliance issues, or audits.
What Are Inpatient Billing Codes?
Inpatient billing codes are standardized codes used to bill for services provided to patients who are formally admitted to a hospital for at least 24 hours. These codes are part of a structured medical coding system that documents every aspect of patient care—from diagnoses and procedures to length of stay and comorbid conditions.
The primary coding systems used in inpatient settings include:
- ICD-10-CM (International Classification of Diseases, Clinical Modification): Used to identify diagnoses.
- ICD-10-PCS (Procedure Coding System): Used for coding inpatient procedures.
- MS-DRGs (Medicare Severity Diagnosis-Related Groups): Classify hospital stays into groups that determine reimbursement levels.
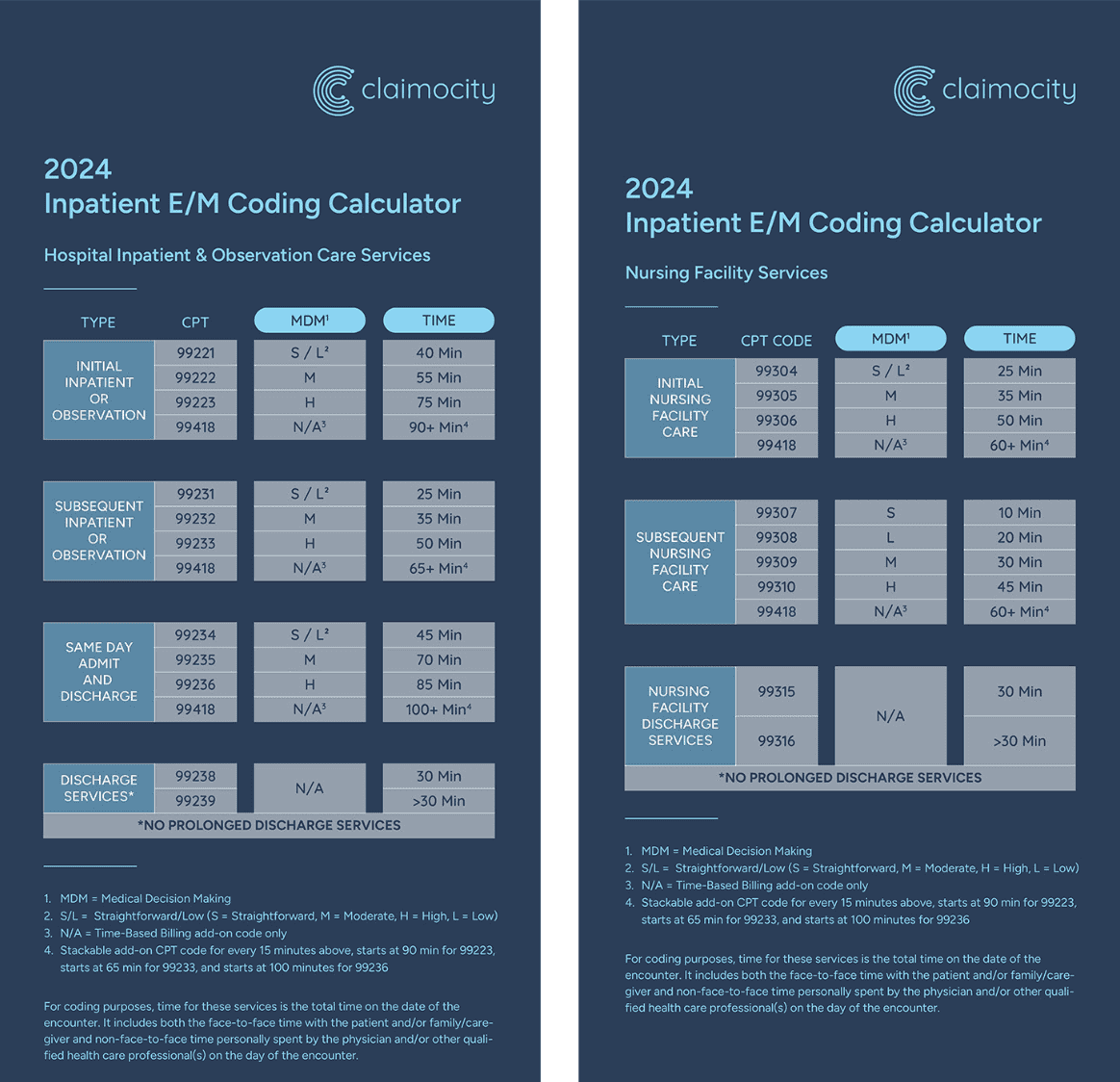
Unlike outpatient billing, which typically uses CPT (Current Procedural Terminology) codes and is billed on a per-service basis, inpatient billing often relies on bundled payment models such as DRGs. This means hospitals are paid a fixed rate based on the patient’s diagnosis and severity level, regardless of the actual services rendered.
Why Inpatient Billing Codes Are So Important
Inpatient hospital stays are among the most expensive services in healthcare. With so much money involved—often thousands or even tens of thousands of dollars per stay—accuracy is essential. Here’s why inpatient billing codes are a critical part of hospital operations:
1. They Drive Reimbursement
DRGs, which are based on inpatient billing codes, directly influence how much a hospital gets paid for a patient’s stay. If a diagnosis or procedure is coded incorrectly or incompletely, the DRG may not reflect the true severity or complexity of the case—resulting in underpayment.
2. They Influence Compliance
Billing errors in inpatient settings are a leading trigger for audits and penalties. Regulatory agencies carefully scrutinize coding practices, and discrepancies can lead to fines or the need to return payments. Accurate coding helps ensure compliance with payer and government rules.
3. They Reflect Patient Complexity
Inpatient billing codes don’t just document services—they tell the story of the patient’s condition. Proper coding of complications, comorbidities, and procedures gives a full picture of the care provided and the resources used.
4. They Support Hospital Performance Metrics
Hospitals use inpatient billing data for more than just billing. The data helps evaluate outcomes, measure provider performance, and benchmark care quality. Accurate coding supports better decision-making and strategic planning.
Challenges of Inpatient Billing
Despite its importance, inpatient billing is far from easy. Hospitals face several hurdles when it comes to using inpatient billing codes effectively:
– Complex Coding Systems
ICD-10-PCS is far more detailed than outpatient CPT coding. Coders need specialized knowledge to select the correct codes from a massive database of procedures.
– Documentation Gaps
Coders rely on providers to document care thoroughly. If documentation is incomplete or vague, it becomes difficult to assign the correct codes, and the hospital risks losing revenue.
– Frequent Code Changes
Billing codes and DRG definitions are updated regularly. Staying current requires ongoing education and system updates.
– High Volume and Pressure
Large hospitals process hundreds or thousands of inpatient claims weekly. Maintaining accuracy under these conditions is a major operational challenge.
Best Practices for Managing Inpatient Billing Codes
To overcome these challenges and protect revenue, hospitals must take a proactive approach to managing inpatient billing. Here are some strategies that make a difference:
1. Strengthen Clinical Documentation
The foundation of accurate coding is clear and complete provider documentation. Hospitals should provide education for physicians on how their notes impact billing and reimbursement.
2. Invest in Certified Coders
Inpatient coding requires expertise. Certified inpatient coders (CICs) are trained in ICD-10-PCS, DRG assignment, and medical terminology. Their accuracy reduces denials and ensures fair payment.
3. Leverage Technology
Coding and billing software can help identify potential errors, suggest appropriate codes, and check claims for compliance before submission. This reduces rework and speeds up payment.
4. Conduct Internal Audits
Routine audits help identify trends in coding errors or documentation deficiencies. This allows for targeted training and process improvements before issues become systemic.
5. Encourage Collaboration
Coders, clinicians, and billing teams must work closely. Open communication ensures that coders can get clarifications, and clinicians understand how their documentation impacts the hospital financially.
Final Thoughts
In the high-stakes environment of hospital finance, inpatient billing codes are more than just numbers. They are the financial translation of complex, life-saving care. Done right, they support fair reimbursement, regulatory compliance, and better data for decision-making. Done wrong, they lead to missed revenue and increased scrutiny.
As healthcare evolves and the demand for value-based care grows, mastering the use of inpatient billing codes will only become more important. Hospitals that prioritize accuracy, invest in the right tools and people, and foster collaboration between teams will be best positioned to thrive—both financially and clinically.