Today, I wish to share with you the transformative potential of insulin pumps – devices that are truly revolutionizing diabetic care.
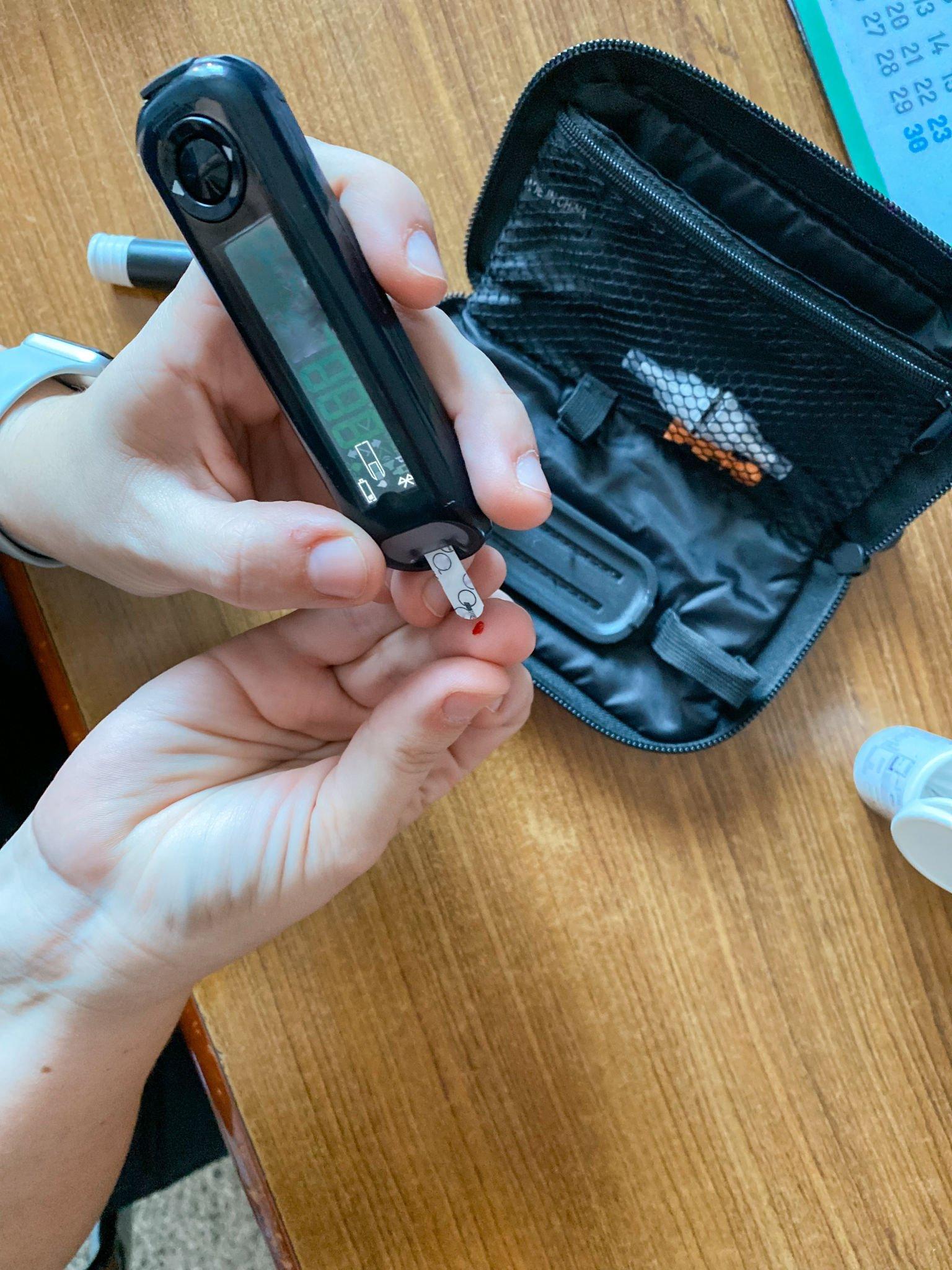
Life with type-1 diabetes isn’t just a medical condition; it’s an intricate dance of routine, resilience, and adaptation. For over 15 years, my mornings and nights have been punctuated with the sting of insulin injections. The constant companion of a glucometer has been there, ensuring my blood sugar levels are on track. Yet, amidst the challenges, the landscape of diabetes management has evolved profoundly.
Understanding Diabetes and the Need for Insulin:
Diabetes is a chronic condition where the body’s ability to produce or respond to the hormone insulin is compromised, leading to elevated blood sugar levels(hyperglycemia).
The main types of diabetes are :
- Type-1 Diabetes
- Type-2 Diabetes
- Gestational Diabetes
Insulin is made by beta cells of pancreas whose function is to transport glucose from the bloodstream into the cells, providing them with the energy they need. Without proper insulin management, glucose remains in your bloodstream resulting in high blood sugar.
With Type-1 diabetes the body does not make any insulin at all hence insulin needs to be injected regularly to lead a healthy life.
Traditional Methods of Insulin Delivery:

The progress of methods of insulin delivery has been very significant over the years from vials and syringes to modern insulin pens.
- SYRINGES – Single use. Less convenient
- INSULIN PENS – Both disposable and reusable are available in the market. Disposable ones come with prefilled cartridges and once insulin is over you can discard the pen whereas reusable one requires the insertion of a 3ml insulin cartridge.
- INSULIN PUMPS
These methods, although effective, often require multiple daily injections and rigorous monitoring, making diabetic management a challenging task for many.
What are Insulin Pumps?

An insulin pump is a small, computerized device about the size of a small cell phone that holds a reservoir of insulin and is worn outside the body. It delivers doses of insulin on a pre-programmed schedule mimicking the way a healthy pancreas delivers insulin to the body.
The pump can be worn:
- Attached to a strap under your clothes.
- In your pocket.
- On your belt.
- With an adhesive patch on your stomach or arm.
How Do They Work?
An insulin pump delivers insulin in one of two ways:
- Small, continuous insulin doses (basal insulin).
- Surges of insulin near mealtimes (bolus insulin).
Constant monitoring of blood sugar levels is still necessary while you are using a pump. Now with Continuous Glucose Monitor(CGM), constant pricking is not needed.
While using an insulin pump, you still need to check your blood sugar levels. Most people check blood sugar at least four times a day. Or you may use a continuous glucose monitor.
The pump uses information you enter about your food intake and blood sugar levels to calculate how much bolus insulin you need. The pump then recommends a bolus dose to you and waits for your approval before delivering. In addition, some pumps automatically adjust basal doses based on glucose levels from a continuous glucose monitor.
Benefits of Using Insulin Pumps for Diabetes Management:
- Consistent Insulin Delivery: It ensures a continuous flow of insulin, eliminating the peaks and troughs often seen with multiple daily injections.
- Flexibility: Whether you’re exercising, sleeping, or indulging in a treat, insulin pumps can be adjusted to cater to different activities and dietary changes.
- Fewer Needle Sticks: Say goodbye to the frequent pricks! With an insulin pump, users only need to change the infusion set every few days.
Choosing the Right Pump for Your Needs:
Just as diabetes management is personal, so is the choice of an insulin pump. When considering a pump, think about its size, features, cost, and user reviews. Consulting with your healthcare provider is essential to make an informed decision.
Some of the best insulin pumps available in the market today are:
- Best with a continuous glucose monitor (CGM): Medtronic MiniMed 630G System
- Best with an exercise setting: Medtronic MiniMed 770G System
- Best tubeless device: Omnipod Dash
- Best slim design: t:slim X2
- Best for portability: Dana Diabecare IIS
- Best for connectivity: Roche Accu-Chek
How to Use an Insulin Pump Effectively:
To get the maximum output from an insulin pump you need to familiarise yourself with many factors like:
1. Training and Setup:
- Get trained by a diabetes educator or doctor.
- Learn how to attach the infusion set to your body.
- Understand how to change insulin in the pump.
2. Troubleshooting:
- Know how to troubleshoot device problems.
- Learn how to change the infusion set.
3. Pump Features:
- Familiarize yourself with the pump’s features.
- Utilize the bolus dose calculator for carb-based insulin needs.
- Consider using “extended bolus” to prevent low blood sugar.
4. Insulin Management:
- Follow the manufacturer’s insulin replacement guidelines.
- Change the infusion site every 2-3 days to maintain effectiveness.
5. Your Role in Diabetes Care:
- Continue regular blood sugar checks.
- Manage your diet.
- Input insulin doses as needed into the pump.
Overcoming Challenges and Common Misconceptions About Insulin Pumps
Common misconceptions associated with insulin pumps are:
- Insulin pumps are complicated and hard to use.
- Infusion sets are uncomfortable or painful.
- Insulin pumps are too expensive.
- Insulin pumps restrict activities or fashion choices and they can disrupt daily routines.
- Pumps increase the risk of low blood sugar.
- Pumps may deliver inaccurate insulin doses.
- Pumps only work with certain insulin formulations.
By being well-informed and seeking guidance, one can easily overcome these challenges and harness the full benefits of the device.
Insurance Coverage and Affordability of Insulin Pumps:
With technological advancement often comes cost. The cost of an insulin pump is generally covered by private health insurance for people with type 1 diabetes (a waiting period applies). Disposable extras required for use (such as cannulas, lines, and reservoirs) are subsidized by the National Diabetes Service Scheme (NDSS).It’s advisable to check with your insurance company for specifics.
In India at present, insulin pumps are usually not reimbursable or covered by insurance, and the patient needs to buy the pump and consumables, both of which are currently expensive. The cost of the pump is a one-time expense, but the cost of the consumables is a recurring expenditure.
Success Stories: Real-life Experiences with Insulin Pumps:
Across the globe, countless individuals have found a renewed sense of freedom and improved health outcomes with insulin pumps. Their testimonies stand as a beacon of hope and an endorsement of this remarkable device. To know more about the success stories with insulin pumps this study can help you.
Embracing the Future of Diabetes Care with Insulin Pumps
Diabetes, once a condition that signified restriction, is being redefined. Insulin pumps, with their promise of flexibility, accuracy, and freedom, represent the pinnacle of this transformation. As we stand at this juncture, looking forward to a future with better diabetes management, it’s clear that pumps are not just a technological marvel but a beacon of hope for millions like me.